How biological timing collides with early schedules and drains daily energy
For many people, mornings feel like a constant uphill battle. Waking up early feels unnatural, mental clarity arrives late, and peak productivity seems to come only after most of the day has already passed.
In a world built around early schedules, this struggle is often framed as a lack of discipline or motivation. In reality, it is usually the result of a mismatch between biological timing and social expectations. For night owls, the problem is not effort — it is alignment.
What It Means to Be a Night Owl
Being a night owl is not a personality trait or a lifestyle choice. It reflects a later biological timing of the sleep–wake cycle, known as a delayed chronotype.
Night owls naturally feel more alert later in the day and evening. Their brains take longer to fully transition into wakefulness in the morning, while cognitive performance, focus, and creativity tend to peak in the afternoon or evening hours.
This pattern is driven by internal biological processes, not habits or preferences. Even when night owls follow early schedules for years, the underlying timing often remains the same.
Why Mornings Feel So Difficult for Night Owls
For night owls, early mornings occur during a biological low point.
At this time, alertness is still rising, reaction time is slower, and mental clarity is reduced. Tasks that require focus, decision-making, or learning demand significantly more effort than they would later in the day.
This is not because the brain is incapable, but because it is being asked to perform before it is biologically ready. The result is a sense of mental fog, heavy fatigue, and resistance to waking that feels disproportionate to the situation.
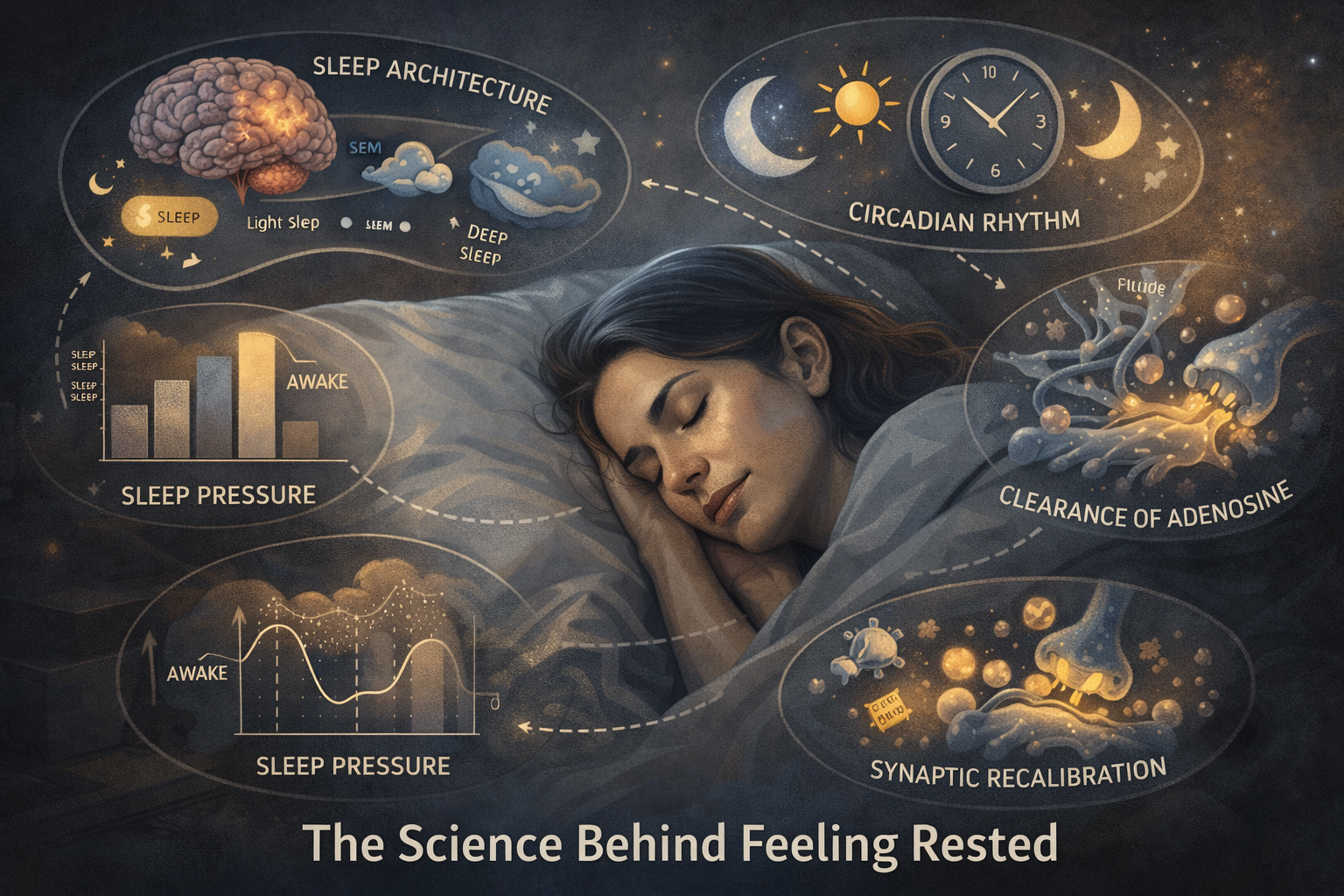
The Role of Circadian Timing
The struggle night owls experience is rooted in circadian timing.
In later chronotypes, the internal clock is shifted forward. Hormonal signals that promote alertness rise later, while signals that promote sleep persist longer into the morning. This delay affects not only sleep onset but also daytime cognitive performance.
When external schedules force early wake-ups, the brain operates out of phase with its internal timing. Over time, this creates chronic misalignment rather than adaptation.
Why Modern Schedules Amplify the Problem
Modern society strongly favors early timing. Work schedules, school start times, and social norms are largely built around morning-oriented chronotypes.
For night owls, this means repeated exposure to early demands combined with insufficient alignment opportunities later in the day. Evening alertness is often cut short by early bedtimes that do not match biological readiness for sleep.
Artificial lighting, evening screen exposure, and irregular routines further complicate the picture, reinforcing delayed timing while simultaneously penalizing it.
The Cognitive Cost of Chronic Misalignment
When night owls are consistently forced into early schedules, the effects accumulate.
Sleep becomes shorter or less efficient. Morning grogginess intensifies. Focus and memory suffer. Emotional regulation becomes more difficult, and perceived stress increases.
Importantly, these effects can persist even when total sleep duration appears adequate. The issue is not simply sleep quantity, but timing misalignment between the brain and the environment.
Over time, this misalignment can lead to chronic fatigue and reduced cognitive resilience.
Why Willpower Doesn’t Solve the Problem
Many night owls attempt to overcome morning struggles through discipline: earlier alarms, stronger coffee, stricter routines.
While these strategies can temporarily mask symptoms, they do not correct the underlying timing mismatch. The brain must expend additional effort to function during biologically suboptimal hours, increasing mental strain rather than improving performance.
Biological timing systems do not respond quickly to motivation. They adapt slowly to consistent cues, not pressure.
Can Night Owls Adapt to a Morning World?
Night owls can make partial adjustments, but full adaptation is uncommon.
Light exposure, routine consistency, and sleep timing can shift the internal clock slightly earlier. However, the fundamental chronotype often remains stable. Large forced shifts frequently result in ongoing misalignment rather than true adaptation.
Understanding this limitation reframes the challenge. The goal is not to become a morning person, but to reduce the friction between biology and daily demands where possible.
Reducing the Impact of Morning Misalignment
Awareness is the first step toward improvement.
Recognizing that morning difficulty is biological rather than personal allows night owls to adjust expectations, protect critical tasks for later hours when possible, and reduce unnecessary self-blame.
Even small timing accommodations can significantly improve perceived energy, focus, and emotional stability. Alignment, not force, is the key.
The Core Idea to Remember
Night owls do not struggle because they lack discipline. They struggle because their biology operates on a later schedule in a world built for early timing.
When the brain is repeatedly forced to perform outside its natural window, fatigue and frustration follow. Understanding this timing mismatch provides clarity — and clarity is the first step toward working with biology instead of fighting it.