Why You Wake Up Before Your Alarm
How circadian timing, stress, and anticipation trigger early awakenings
Waking up before your alarm can feel confusing or frustrating. Sometimes it happens once and feels harmless. Other times it becomes a pattern — early mornings, alertness too soon, and difficulty falling back asleep.
This experience is rarely random. Waking before the alarm is often a sign that the brain has already transitioned toward wakefulness. The reason lies in how circadian timing, stress systems, and learned anticipation interact during the final hours of sleep.
The Brain Wakes Up Before the Alarm Does
Waking up is not caused by the alarm itself.
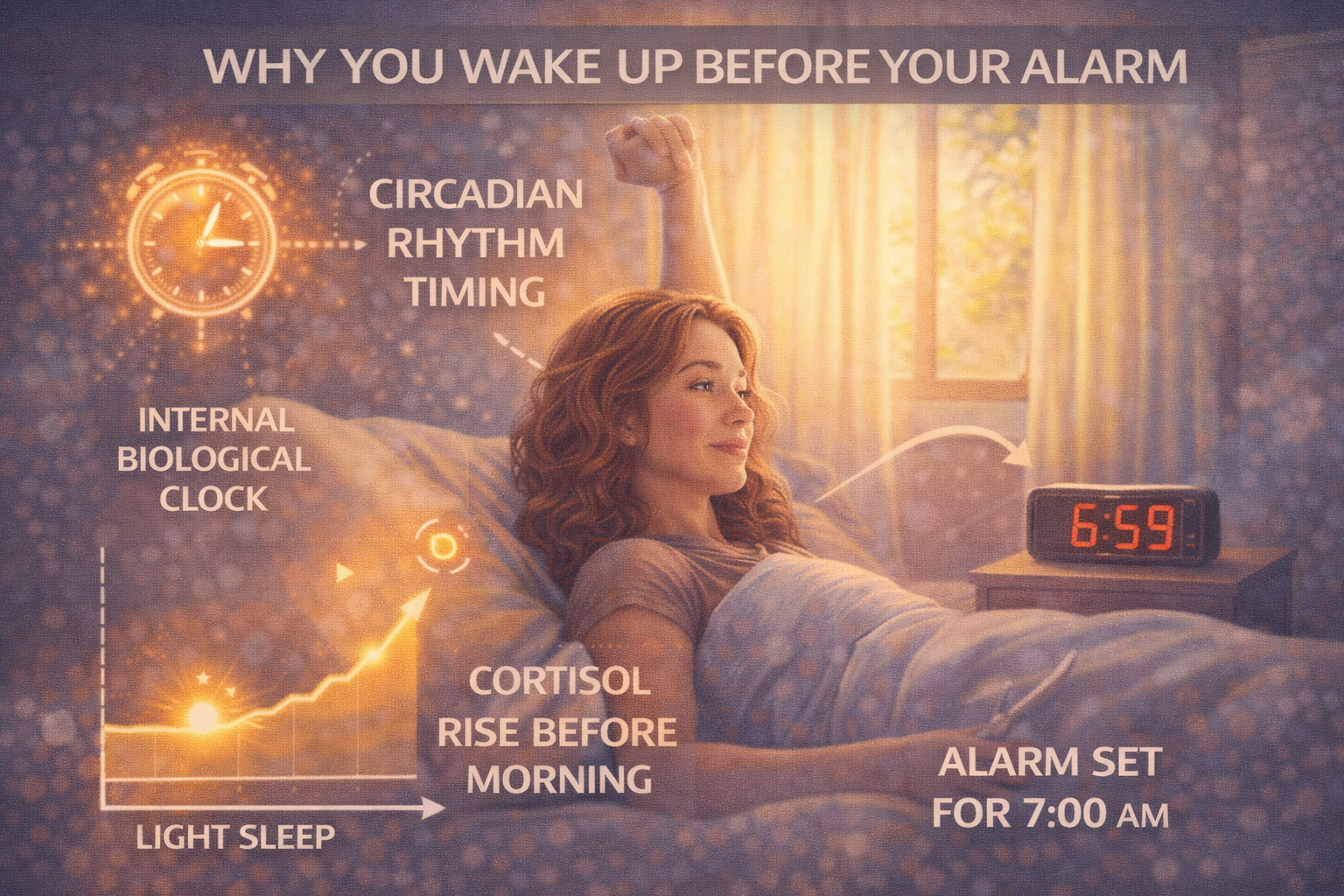
The brain begins preparing for wakefulness well before morning. Hormones shift, body temperature rises, and alertness gradually increases as part of the circadian rhythm.
If this transition reaches a certain threshold before the alarm goes off, you wake naturally — sometimes minutes, sometimes much earlier.
Circadian Rhythm and Early Wake Signals
The circadian rhythm determines when the brain expects the day to begin.
If your internal clock is shifted earlier than your alarm time, wake-promoting signals may rise sooner than intended. This can happen due to consistent early schedules, light exposure, or gradual shifts in sleep timing.
In these cases, waking before the alarm is a sign of circadian alignment — not necessarily a problem.
Stress and the Early Morning Alert Response
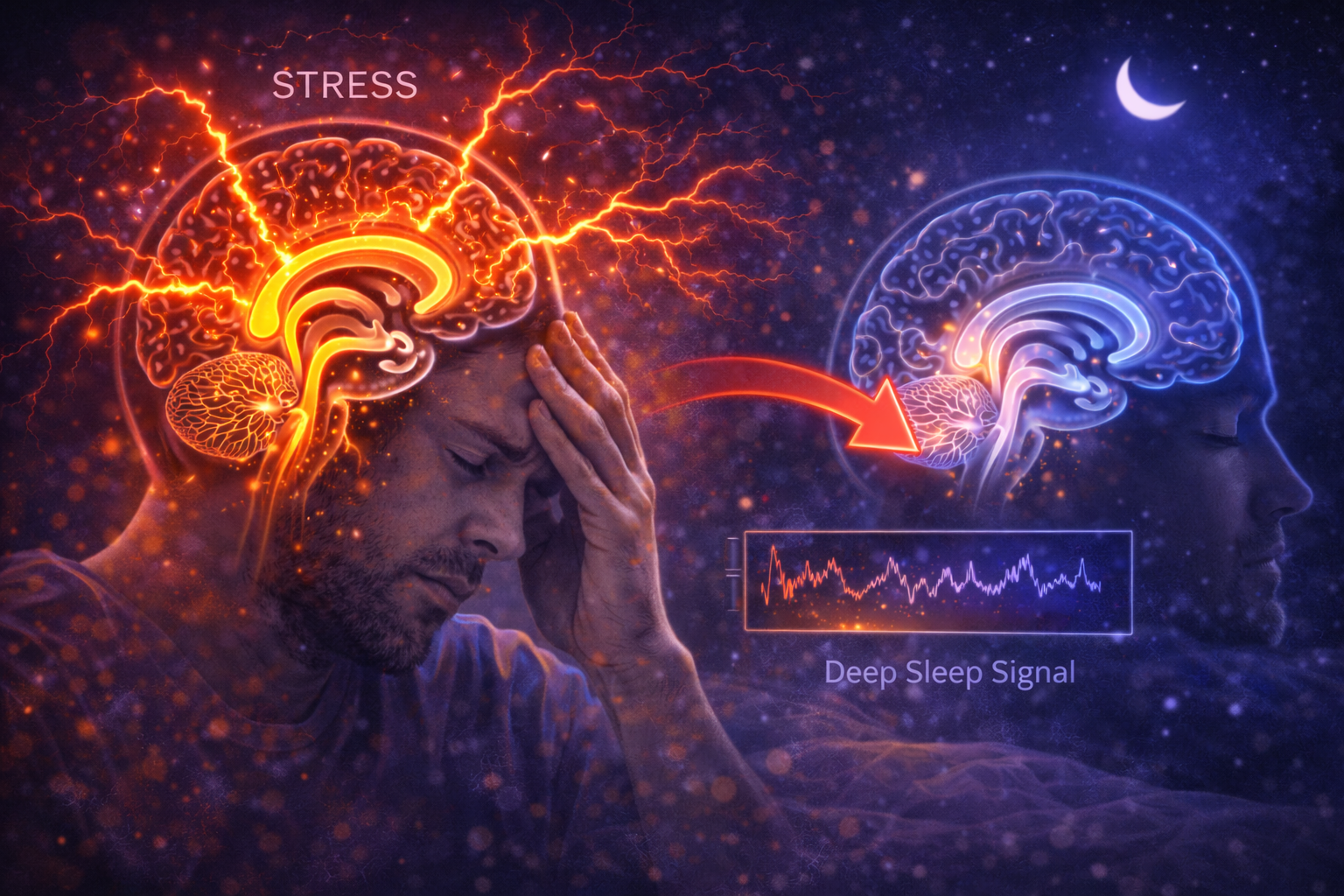
Stress is a common cause of unwanted early awakenings.
Stress hormones naturally rise in the early morning to support waking. When stress levels are elevated, this rise can occur earlier or more intensely, triggering premature alertness.
Even low-grade or subconscious stress can activate the brain before the desired wake time.
Why Anticipation Wakes You Up
The brain learns patterns quickly.
If you regularly wake at a certain time, worry about waking early, or anticipate an upcoming obligation, the brain begins preparing earlier. This learned anticipation can override sleep continuity.
As a result, the brain exits sleep not because rest is complete, but because it expects action.
Sleep Pressure Is Lowest in the Morning
Sleep pressure decreases across the night.
By early morning, sleep pressure is naturally lower than at bedtime. This makes sleep more fragile and easier to interrupt.
When combined with rising circadian alertness or stress signals, even small disturbances can cause full awakening.
Why Falling Back Asleep Is Hard
Once the brain transitions toward wakefulness, returning to sleep becomes difficult.
Alertness systems activate quickly, while sleep-promoting systems take longer to re-engage. The brain interprets early waking as the start of the day, even if the alarm has not sounded.
This imbalance explains why early awakenings often end the night entirely.
Early Waking and Sleep Fragmentation
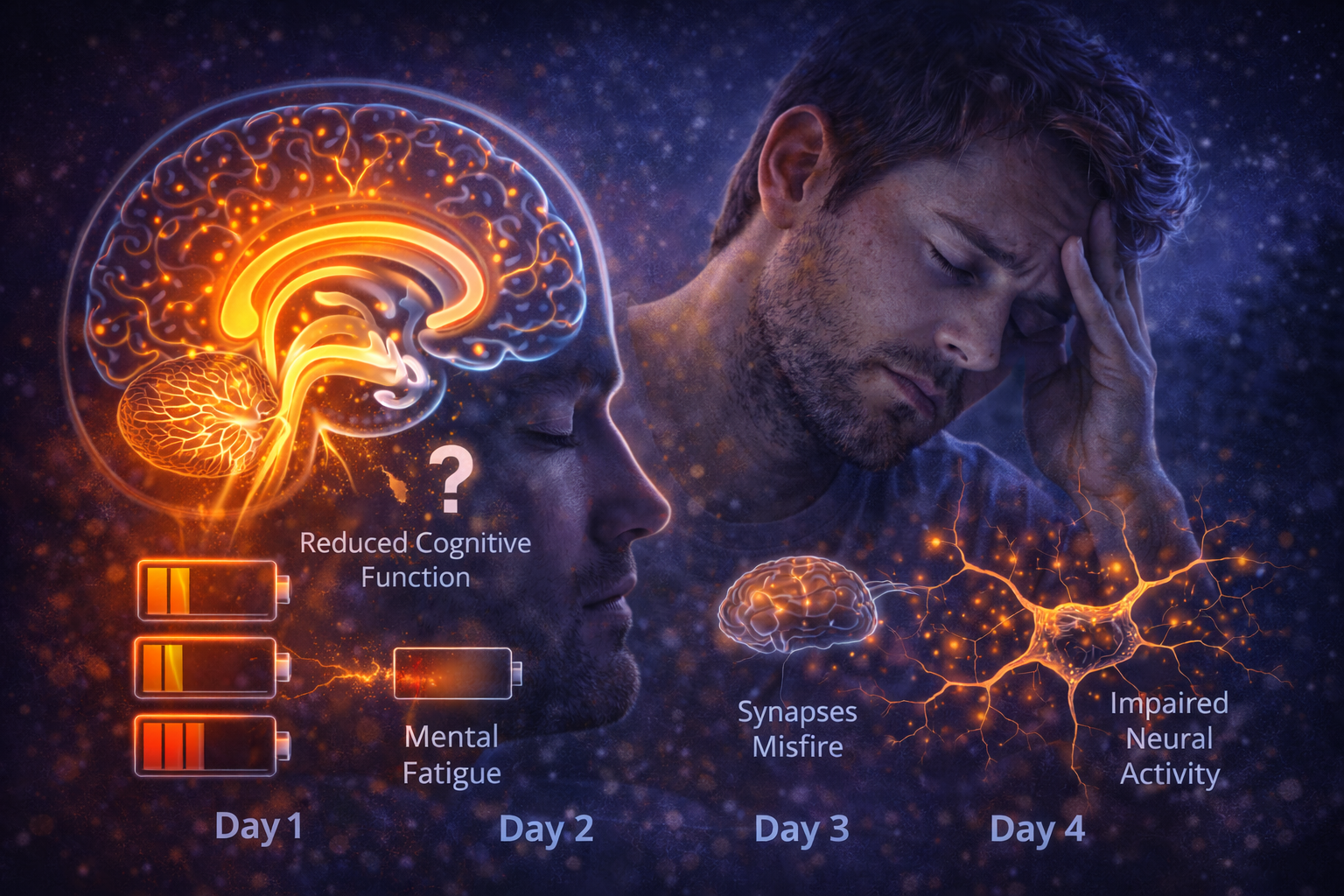
Frequent early awakenings fragment sleep.
While total sleep time may not appear drastically reduced, the final and often REM-rich portion of sleep is shortened. This can affect emotional processing and leave sleep feeling incomplete.
Repeated early waking contributes to cumulative fatigue over time.
Why Sleeping Earlier Doesn’t Always Help
Many people respond to early awakenings by going to bed earlier.
If circadian timing does not shift accordingly, this strategy increases time in bed without extending sleep. The brain still wakes at the same internal time.
Timing alignment matters more than bedtime alone.
When Early Waking Is Actually Normal
Not all early awakenings are negative.
If you wake feeling alert, rested, and calm, early waking may simply reflect a well-aligned circadian rhythm. Problems arise when early waking is accompanied by fatigue, anxiety, or sleep loss.
The context determines whether the pattern is healthy or disruptive.
Reducing Unwanted Early Wake-Ups
Improving early waking often involves reducing early-morning alert signals.
Supporting circadian alignment, managing stress, and protecting sleep continuity help the brain maintain sleep through the final hours. The goal is not forcing sleep, but preventing premature activation.
When the brain stays in recovery mode longer, sleep naturally extends closer to the alarm.
The Core Idea to Remember
Waking up before your alarm happens because the brain has already begun waking.
Circadian timing, stress hormones, anticipation, and low sleep pressure combine to trigger early alertness. This process is biological, not random.
Understanding why it happens helps distinguish healthy early waking from patterns that undermine sleep — and points toward alignment rather than effort as the solution.