What blue light blocking can and cannot do for your sleep
Blue light blocking glasses, screen filters, and “night mode” settings are widely promoted as simple solutions for sleep problems. Many people use them hoping to fall asleep faster and sleep more deeply.
But the reality is more nuanced. Blue light blocking can help—but it is not a complete fix. Its effectiveness depends on timing, behavior, and expectations. Understanding what blue light blocking actually does clarifies when it works and when it doesn’t.
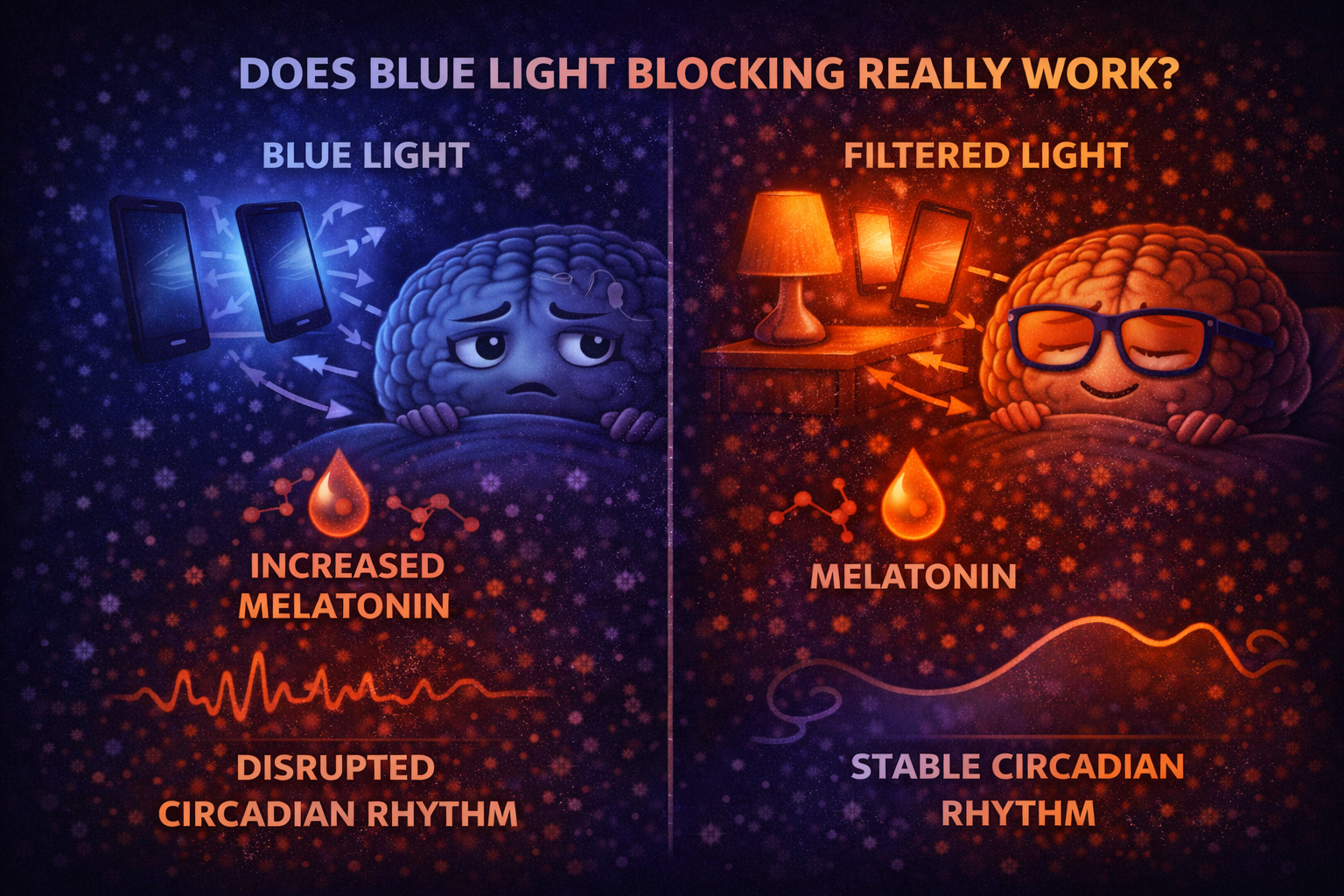
Why Blue Light Blocking Exists
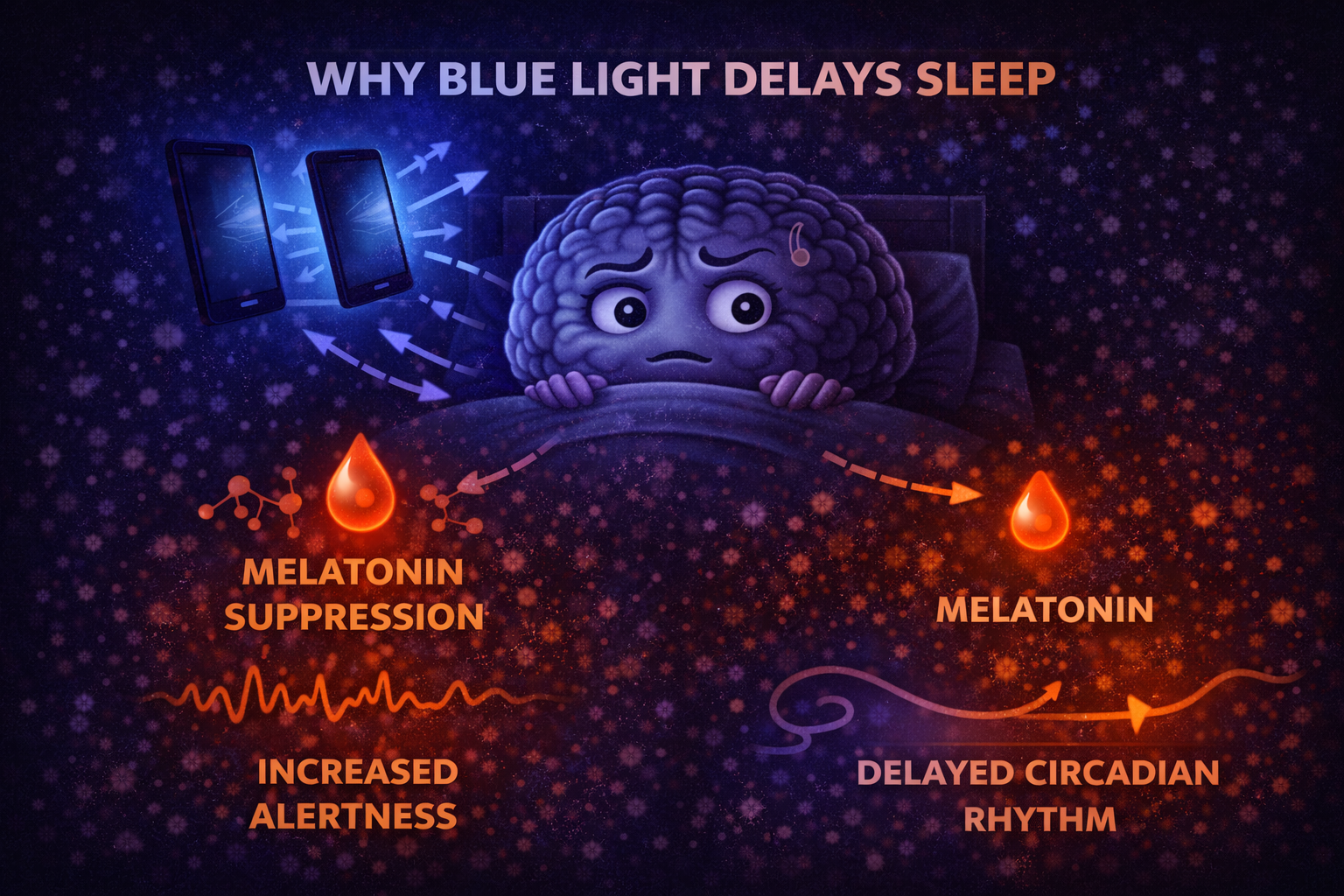
Blue light delays sleep by signaling daytime to the brain.
Blocking blue wavelengths reduces melatonin suppression and limits circadian delay. This is the biological rationale behind blue light blocking tools.
They are designed to weaken one specific signal—not to replace healthy sleep habits.
What Blue Light Blocking Does Well
Blue light blocking reduces one major disruptor.
By filtering blue wavelengths, these tools decrease the alerting signal sent to the brain in the evening. This can support earlier melatonin release and make sleepiness feel more natural.
For people exposed to screens at night, this reduction can be meaningful.
Why Blue Light Blocking Is Not a Complete Solution
Blocking blue light does not eliminate alertness.
Brightness, screen content, mental stimulation, and timing still affect sleep. Even filtered light can delay sleep if exposure is long or intense.
The brain responds to more than just wavelength.
Screens Still Stimulate the Brain
Visual content matters.
Reading messages, watching videos, or engaging emotionally activates cognitive and emotional systems regardless of light color. This stimulation delays sleep independently of blue light.
Blue light blocking does not prevent mental arousal.
How Effective Are Blue Light Blocking Glasses?
Glasses can reduce circadian disruption—but with limits.
They are most helpful when worn consistently in the evening and combined with dim lighting. Their effect is smaller if screens are used intensively late at night.
They work best as a support, not a solution.
What About Screen Night Modes and Filters?
Software filters help—but partially.
Night modes reduce blue wavelengths but often maintain brightness and contrast. This still stimulates the visual system and the brain.
Reducing screen time matters more than adjusting screen color alone.
Why Timing Matters More Than Filtering
Light timing is more important than light filtering.
Blocking blue light late at night helps less than reducing exposure earlier in the evening. Prolonged exposure—even filtered—can still delay sleep.
The circadian system responds to cumulative signals.
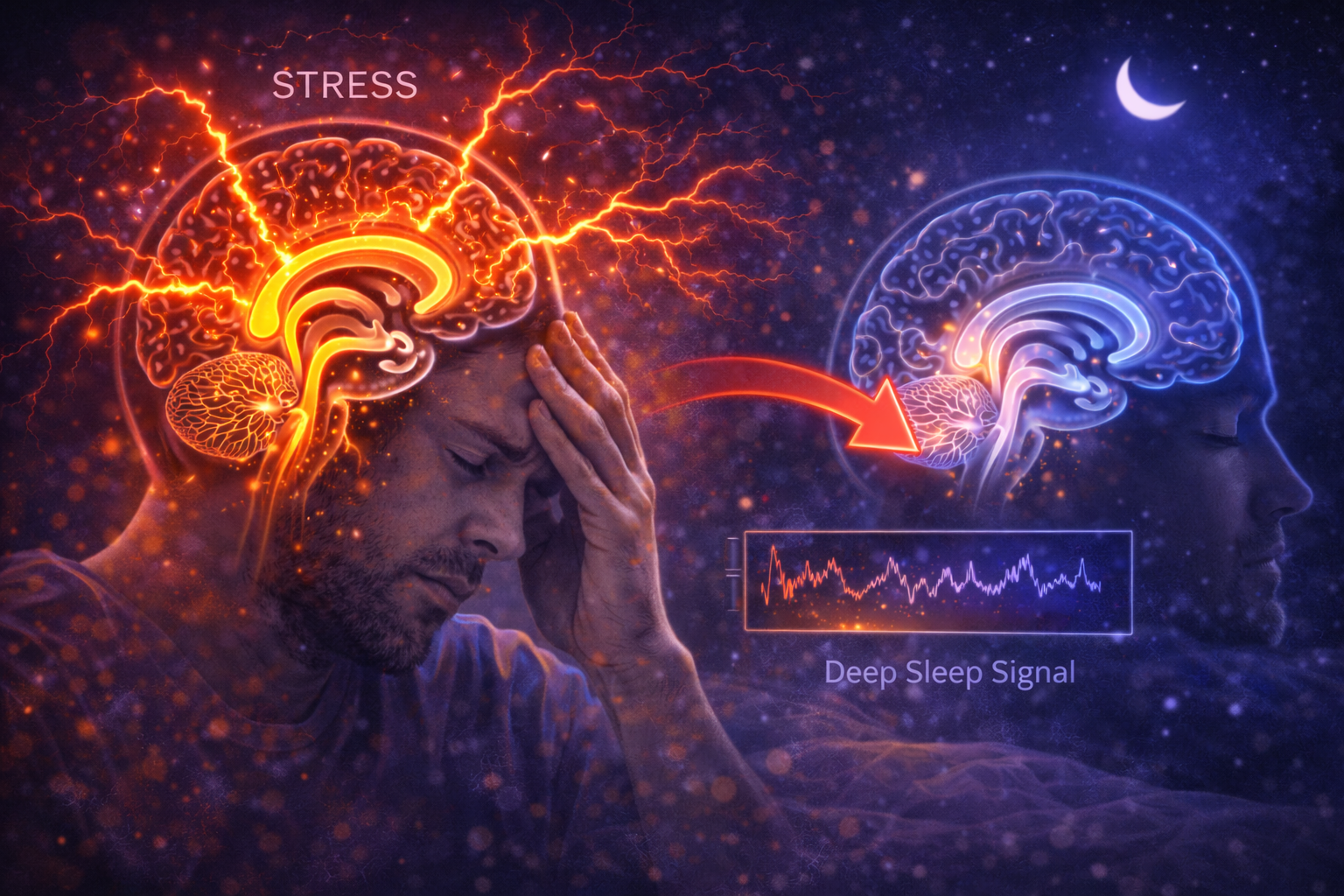
Blue Light Blocking and Sleep Quality
Blue light blocking mainly affects sleep timing.
It may help you fall asleep earlier but does not guarantee deeper sleep. Sleep depth depends on overall circadian alignment, stress levels, and sleep continuity.
Blocking blue light improves conditions—but doesn’t replace biology.
When Blue Light Blocking Is Most Useful
It works best when:
-
evening screen use is unavoidable
-
lighting is already dim
-
bedtime is consistent
-
exposure time is limited
In these conditions, blue light blocking can meaningfully support sleep.
When Blue Light Blocking Has Little Effect
It helps less when:
-
screens are used intensively late at night
-
lighting is bright
-
sleep timing is irregular
-
stress and arousal remain high
In these cases, behavior matters more than filtering.
The Bigger Picture: Light Management
Blue light is only part of the story.
Sleep improves when light exposure is aligned across the entire day—bright mornings, dim evenings, consistent timing.
Blocking blue light without managing overall light habits has limited impact.
The Core Idea to Remember
Blue light blocking works—but only within limits.
It can reduce melatonin suppression and support earlier sleep onset, but it does not eliminate alertness, stimulation, or poor sleep habits.
Blue light blocking is a tool—not a cure. Sleep improves most when light exposure, timing, and behavior work together.